ABA Therapy Insurance Coverage for Autism (By State)
Find out which autism insurance providers cover ABA therapy and more in this guide. This is the only autism insurance guide you'll need.

Is ABA therapy covered by insurance?
The good news is ABA therapy is most likely covered by your insurance plan. In fact, most insurance plans will cover autism therapy, including ABA therapy and autism evaluations. Coverage varies based on your location and plan, so it's important you check with your provider.
We welcome you to contact our support team to verify your insurance coverage for ABA therapy.
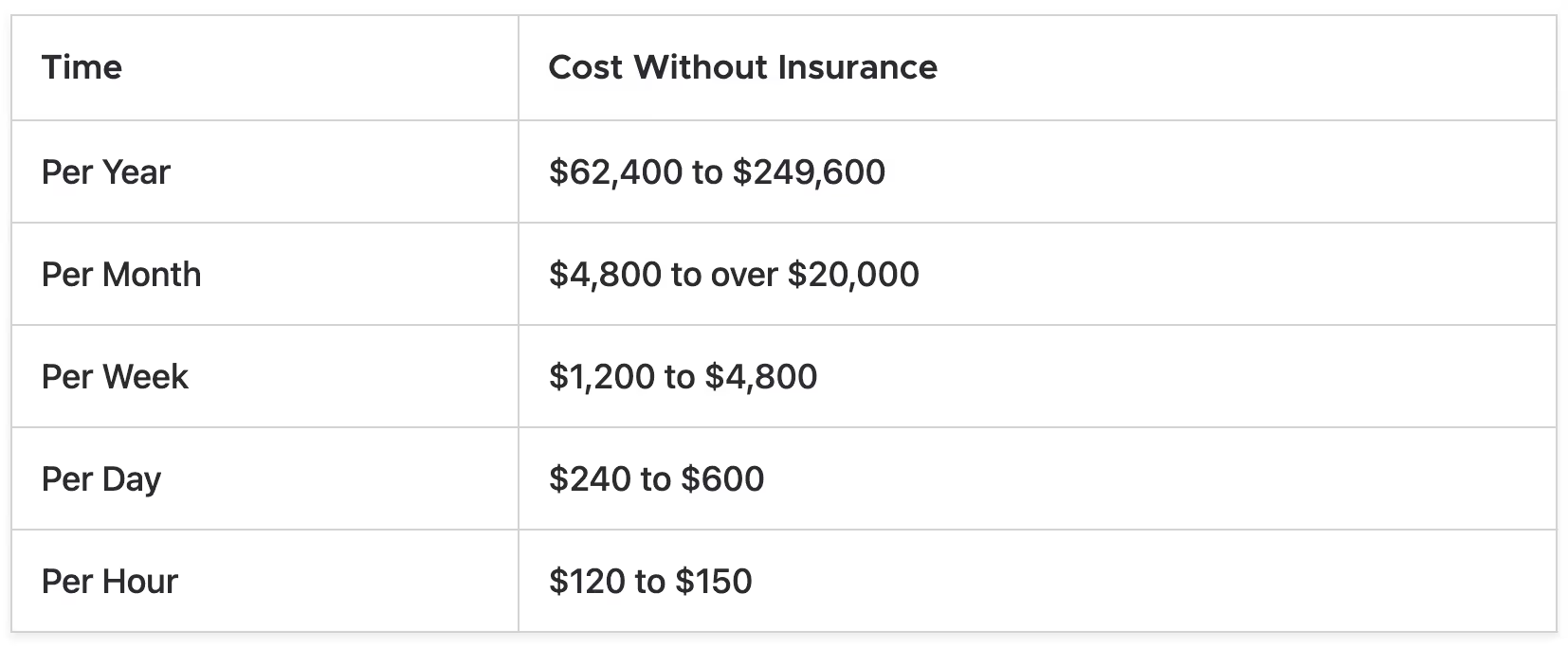
How much does ABA therapy cost without insurance?
ABA therapy costs $62,400 to $249,600 per year without insurance coverage.
The monthly costs for ABA therapy can range from $4,800 to over $20,000 per month without insurance coverage.
ABA therapy weekly costs start at $1,200, and can go up to $4,800 without insurance coverage.
However, don't let these prices scare you, your insurance provider most likely covers these costs. The chart below shows how much insurance pays for ABA therapy:
How do insurance companies cover ABA?
Your coverage for ABA can vary from state to state, and from plan to plan. Some insurance companies are quick to cover ABA, but others are much more conservative in their coverage. Every insurance plan comes with a booklet that explains the plan's coverage.
However, the terminology and language used is technical and can be hard to understand.
But don't give up, dig in, and you should find information about whether or not your plan covers Applied Behavior Analysis.
If you don't see that information, or you're not sure how to interpret the plan, call the customer service number listed on your membership card and ask the insurance company's support team. The chart below will explain how insurance companies cover ABA.
Here is a breakdown of comparing plans side by side:

Insurance ProviderDescriptionMedicaidAs of February 2022, all 50 states have implemented Medicaid insurance coverage for autism treatment. Read our Medicaid insurance coverage guide to learn more.CignaSome plans cover ABA. If you have a Cigna plan, your doctor must submit formal ASD diagnosis paperwork before therapy begins.Blue Cross Blue ShieldEvery plan is different under this label. For example, ABA is covered for people younger than 18 in Michigan. Some plans require preauthorization or paperwork before therapy begins.Kaiser PermanenteKaiser was the first company in Oregon to voluntarily cover ABA in 2012. However, not all states offer that coverage. For example, some plans don't include coverage in Washington.AetnaAetna does not explicitly cover ABA therapy, but it could be allowed. Speak with the company about if you could qualify for coverage.
Important insurance terms
If your child is diagnosed with autism, and you're searching for autism treatment, it's important you understand common insurance terms that will come up throughout the treatment process.

HealthCare.gov has a complete glossary of insurance terms that every parent should know. Here are just a few that might be helpful to know:
- Deductible: A deductible is different than a premium; it's the amount you pay for out-of-pocket costs for your covered health care before your benefits kick in.
- Copayment or coinsurance: This is what you are expected to pay after the insurance provider pays a bill.
- Out-of-pocket maximum: This is the maximum amount you can expect to pay out of pocket every year for covered autism treatment services. This includes deductibles, copayments and coinsurance. However, premiums are not factored into this amount.
- Prior authorization: It's a health plan cost-control process by which health care providers must obtain approval from a health plan before a specific service is delivered to the patient to qualify for coverage.
- Network: Your network is made up of providers and professionals with contracts with your insurance provider. If you step out of that network, for whatever reason, you could pay a larger portion of your bill, or the entire amount.
- PPO: This acronym is short for "preferred provider organization". You have a network of professionals to choose from. You also have access to some benefits even if you step outside the network.
- HMO: This acronym is short for "health maintenance organization", and it's where you have a network of providers you must use to have the ability to access insurance benefits.
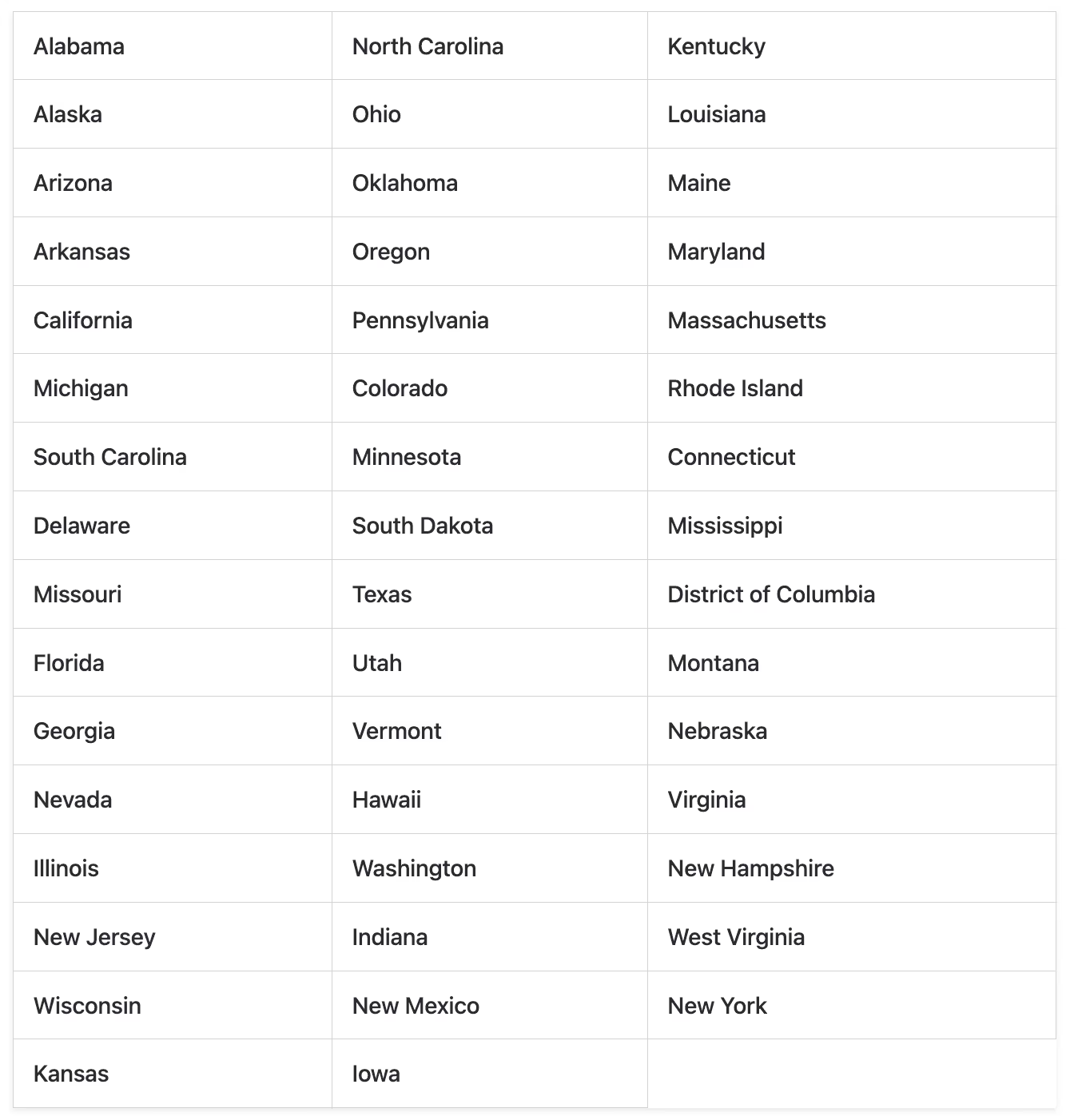
Autism insurance coverage by state
The American Speech-Language-Hearing Association compiled data on a list of states. Here is a sample list:
- California: If a plan covers physical treatments, that plan must also cover mental health services. The good news is ABA therapy is considered a covered autism treatment.
- Indiana: ABA therapy isn't explicitly covered here, but therapy for autism and related disorders may not be subject to limits or deductibles.
- Georgia: ABA therapy isn't explicitly covered here.
- Montana: ABA isn't explicitly mentioned. Autism treatments can be capped at $50,000 per year for children 8 years old or younger.
- Arkansas: ABA therapy is covered when provided by a board-certified and supervised expert.
The following states have specific autism mandates, which require certain insurers to provide coverage for autism spectrum disorder.
Insurance companies that cover ABA therapy
Here are some of the most well-known insurance companies that can cover the costs of ABA therapy.
If you're looking for the best health insurance for ABA therapy, the list below should be valuable. Visit the links attached to learn more about each insurance company's coverage for autism treatment.
- Medicaid -> Read More
- Aetna -> Read More
- Cigna -> Read More
- UnitedHealthCare -> Read More
- BlueCrossBlueShield -> Read More
- Kaiser Permanente -> Read More
- Anthem -> Read More
How many people have ABA therapy covered by health insurance?
At least 200 million people now have health insurance coverage for ABA therapy. Over the last decade, AutismSpeaks.org's advocacy team has focused their efforts on improving health insurance coverage for medically necessary treatments such as ABA.
Read More: Financial Assistance For Autism
Self-funded vs. fully funded ABA therapy insurance plans
Laws surrounding insurance plans can get confusing. For example, AutismSpeaks.org says there are two types of insurance plans in the United States, with fundamentally different coverage types. You might not know what type of plan you have, and that's okay. Many people don't, but there are tools that can help you find out.
- Self-funded plans: A self-funded plan must comply with federal laws, but not the state versions. Your employer makes the final decision about what will and won't be covered by insurance.
- Fully insured plans: A fully insured plan must provide benefits per state laws, and your insurance company will determine what is and isn't covered.
Knowing what type of plan you have will help you understand the benefits you have, what's covered, and will help you have more confidence when choosing an insurance plan to cover autism treatment.
Coverage for ABA therapy might not be explicitly supported by your state, but there is a high chance your state does mandate coverage for autism. In either case, the benefits vary significantly depending on where you live.
Questions to ask your insurance provider
Here are some questions that you can (and should) ask your insurance provider to understand more about how much coverage you have when starting ABA therapy:
- Is ABA therapy covered by my insurance as a benefit for my child?
- How much does my insurance cover ABA therapy?
- How long / how many therapy sessions are allowed?
- What is my coinsurance or copay?
- How old can my child be to receive coverage for ABA therapy?
- What criteria are needed for ABA therapy to be covered?
- Do I need a specific autism diagnosis or paperwork to be filed?
- What is my family or individual deductible for ABA therapy?
- Which specific ABA therapy providers are in-network? Is CrossRiverTherapy covered?
Does insurance cover ABA therapy for ADHD?
Most insurance companies only cover ABA therapy with an Autism diagnosis. Also some insurance carriers will require a letter from your child's treating physician stating why ABA therapy is medically necessary. Therefore, make sure to ask the insurance representative if you will need a letter in order to begin treatment.
Does insurance cover autism testing?
There are some insurance companies which can cover autism testing, but coverage will vary based on your location and plan. Read our guide to insurance for ABA therapy to get a strong understanding of how insurance can cover ABA.
Find More ABA Therapy Insurance Articles
Insurance Coverage For ABA Therapy
Find out which autism insurance providers cover ABA therapy and more in this guide. This is the only autism insurance guide you'll need.
Financial Landscape of Autism: Financial Planning
Autism is a complex condition that affects not only individuals but also families, communities, and society as a whole. In this article, we’ll take a closer look at the financial aspects of autism and how you can navigate them.
ABA Therapy That Accepts Medicaid
We have you covered. CrossRiverTherapy accepts Medicaid for all of our autism therapy services, whether it's at-home, our clinic, or online.
Does Aetna Cover ABA Therapy?
Yes, Aetna covers Applied Behavior Analysis (ABA), but there could be limitations to receiving full coverage.
Does Anthem Cover ABA Therapy?
Yes, Anthem covers ABA therapy under most conditions. Speak with our team to learn if your child's ABA therapy can be covered by Anthem.
Does United Healthcare Cover ABA Therapy?
Yes, United Healthcare provides coverage for behavioral therapies based on ABA principles and other medically essential behavioral regimens.
Does Cigna Cover ABA Therapy?
Find out which autism insurance providers cover ABA therapy and more in this guide. This is the only autism insurance guide you'll need.
Does Blue Cross Blue Shield Cover ABA Therapy?
Yes, Blue Cross Blue Shield covers Applied Behavior Analysis (ABA) therapy for children under 18. Read on to learn about the provider's autism therapy coverage.
Does Humana Cover ABA Therapy?
Yes, Humana covers ABA therapy costs and includes ABA therapy as a part of their insurance plans. Read on to learn the autism treatment Humana covers.
Does Kaiser Permanente Cover ABA Therapy?
Yes, Kaiser Permanente covers ABA therapy costs and includes ABA therapy as a part of their insurance plans.
